corneal thickness is measured by|average corneal thickness range : bespoke Corneal thickness as measured by pachymetry is important in the eye care field for several reasons. Pachymetry can tell healthcare providers if the cornea is swollen. Medical conditions such as Fuch's Dystrophy can increase .
WEB5 de nov. de 2023 · Nos últimos tempos, a Bet60 tem atraído a atenção de muitos entusiastas de jogos online. Com a promessa de entretenimento e, potencialmente, ganhos financeiros, não é de surpreender que as pessoas estejam curiosas sobre a confiabilidade dessa plataforma. Neste artigo, vamos explorar a Bet60, como ela funciona e .
{plog:ftitle_list}
WEBJulia K Barni / juliakbarni / Nude OnlyFans Photo #32. Newer; Older; Popular
A pachymetry test, or corneal pachymetry test, measures the thickness of your cornea. Thickness matters for glaucoma and refractive errors, and if you’re considering eye surgery. How is the thickness of the cornea measured? The thickness of the cornea can be measured using various techniques, including ultrasound pachymetry, optical coherence .
A pachymetry test is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and . To measure the corneal thickness, a special ultrasound can be used called a pachymeter. Additionally, there are instruments that use light waves to form a cross-section of the cornea called an OCT that can be .Normal corneal thickness is about 540 microns (half of a millimeter). Thickness is checked with a handheld ultrasound device called a pachymeter. We check corneal thickness mainly for two . Corneal thickness as measured by pachymetry is important in the eye care field for several reasons. Pachymetry can tell healthcare providers if the cornea is swollen. Medical conditions such as Fuch's Dystrophy can increase .
thin cornea thickness chart
The normal cornea varies in thickness. It is thickest in the periphery at the limbus at around 700–900μm and thinnest centrally at the corneal apex at around 544μm (approximately 1⁄2 a .
Anti-Itch Powder moisture meter
Central corneal thickness (CCT) measurements are commonly used to assess corneal endothelial function and to evaluate patients before and after keratorefractive surgery. . Owing to its general ease of use, repeatability, and modest cost, the most widespread method to measure CCT is ultrasound pachymetry (UP), which requires contact .
Corneal pachymetry is the measurement of corneal thickness, done through a simple, quick, painless test to assit in better understanding ophthalmic issues. To measure the corneal thickness, a special ultrasound can be used called a pachymeter. Additionally, there are instruments that use light waves to form a cross-section of the cornea called an OCT that can be measured to .That’s where corneal topography comes in. This technology allows eye care specialists to map and measure your cornea, including its thickness and elevation changes. Corneal topography is the gold standard for mapping subtle changes in your cornea that occur suddenly or over time. Computerized corneal topography is another name for this test.
We aimed to compare five different devices that measure Central Corneal Thickness. The Central Corneal Thickness (CCT) is an important parameter in ophthalmology. It is involved in the management of various eye conditions such as: glaucoma, keratoconus, contact lens wearing, corneal dystrophies, refractive surgery and keratoplasty.Comparison of central corneal thickness measured by standard ultrasound pachymetry, corneal topography, tono-pachymetry and anterior segment optical coherence tomography. Curr Eye Res. 2018;43:866–72. doi: 10.1080/02713683.2018.1461910. [Google Scholar] 5. Fujioka M, Nakamura M, Tatsumi Y, Kusuhara A, Maeda H, Negi A. Comparison of Pentacam . Corneal imaging is widely used by ophthalmologists to understand the shape and curvature of the cornea. Corneal topography evaluates the anterior surface of the cornea and displays the information using a color-coded map. On the other hand, corneal tomography takes into account the thickness of the cornea, allowing the posterior surface of the cornea to be .The thickness of the cornea was reported in more than 100-year-old textbooks on physiological optics (Helmholtz, Gullstrand). . Several techniques for its measurement have been described and physiological and clinical significance have been studied. In this review, the different methods and techniques of measurement are briefly presented .
Corneal thickness is also an independent risk factor for the development of glaucoma. Central corneal thickness can be easily measured using a handheld ultrasound pachymeter. This article provides an overview of the methods of corneal pachymetry and the interpretation of the results. A boxplot showing the spread of corneal thickness (all eyes) is given in Figure 1. The distribution of corneal thickness by diagnosis is given in Figures 2 through 7, which are drawn to the same scale to aid comparison between the different graphs. The histograms show that the CCT of eyes with a diagnosis of normal, POAG, and GS follow a normal . Corneal thickness measurement (pachymetry): A thin cornea, which increases your risk of primary open-angle glaucoma. Dilated eye exam: Atypical size and shape of blood vessels inside your eye. Eye pressure check: Intraocular (eye) pressure greater than 22 mmHg (millimeters of Mercury).
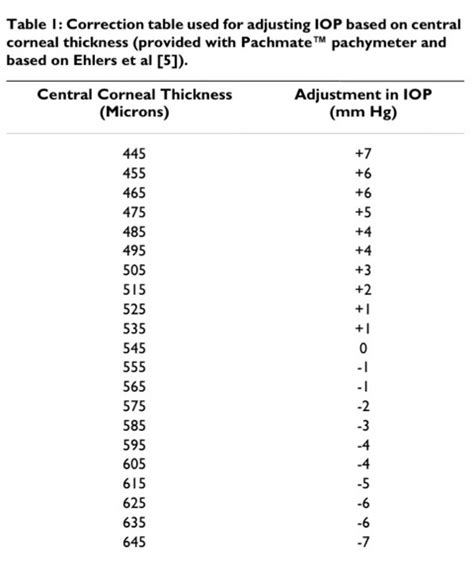
Intraocular pressure measurement is influenced by corneal thickness, among other factors. Eyes with thin corneas tend to have pressures that are under-estimated by tonometry, while eyes with thick corneas tend to have pressures that are over-estimated. Manufacturers of devices that measure corneal thickness (such as the corneal pachymeter) often supply clinicians with . The healthy central cornea is aspheric and prolate (the central curvature is steeper than the periphery).[1] Attempts to measure the cornea were made as early as the 1600s by Scheiner, who compared reflections produced by glass spheres whose diameters were known to the reflections from the anterior surface of the cornea.[2] The central keratometric values vary .
Corneal thickness is usually measured with an ultrasound pachymeter. After your eye is numbed with anesthetic eye drops, the pachymeter probe will be placed in front of your eye, just touching the corneal surface. Measurements are automatically taken by the probe and then displayed on the monitor. There are other instruments that can measure .Another risk factor is corneal thickness, the thickness of the clear outer surface of the eye. The thinner the cornea the higher risk of developing glaucoma. . Many believed that the thickness of the cornea alters the measurement of IOP. There is no question that corneal thickness has an effect on the measurement of IOP; however, the effect .Central corneal thickness (CCT) is a valuable and sensitive measure of corneal health and physiological performance . It can be a crucial factor to consider when monitoring corneal pathologies such as keratoconus, Fuchs’ endothelial dystrophy, and corneal edema [ 2 , 3 ].Measurement of CH also provides a more complete characterization of the contribution of corneal resistance to intraocular pressure measurements than central corneal thickness (CCT) alone. However, corneal hysteresis values can be produced by various combinations of corneal thickness, rigidity, intraocular pressure, and hydration.
Objective: To determine if a single measurement of central corneal thickness (CCT) is an adequate sample to aid in glaucoma risk assessment in clinical practice. Methods: Central corneal thickness was measured by ultrasound pachymetry (mean of 15 measurements for each eye) on two separate occasions at least one month apart (range, 33 to 610 days).Objective: To evaluate published literature to assess whether central corneal thickness (CCT) is a risk factor for the presence, development, or progression of glaucomatous optic nerve damage related to primary open-angle glaucoma (POAG). Methods: A PubMed literature search limited to English language articles conducted on November 15, 2004 retrieved 195 articles.
Intraocular pressure measurement is influenced by corneal thickness, among other factors. Eyes with thin corneas tend to have pressures that are under-estimated by tonometry, while eyes with thick corneas tend to have pressures that are over-estimated. Manufacturers of devices that measure corneal thickness (such as the corneal pachymeter) often supply clinicians with .Central corneal thickness (CCT) is an important parameter that is routinely measured in clinical ophthalmology practice and used in the diagnosis and follow-up of ocular diseases such as glaucoma, keratoconus, and corneal ectasia. 1 However, the accurate measurement of CCT is also used to monitor corneal edema and endothelial function, to plan . To assess the impact of knowing central corneal thickness (CCT) on glaucoma management in a United Kingdom district general hospital. A masked observational non-interventional study included 304 eyes of 152 consecutive glaucoma cases attending general clinic. CCT was measured using a hand-held pachymeter. IOP, as measured by the .At Flaum Eye Institute Refractive Surgery Center, your corneal thickness will be measured first by the Orbscan IIz Corneal Analysis System. This form of measurement gives the doctors an overall view of your corneal thickness across the entire cornea. It also identifies the thinnest point in the cornea, both by value and location.
The measurement of central corneal thickness (CCT) holds crucial significance in the diagnosis and monitoring of numerous ophthalmic diseases, including keratoconus, glaucoma, as well as pre- and post-refractive surgeries. Additionally, it serves as a vital diagnostic tool in the evaluation of endothelial dysfunction, such as Fuch's endothelial .Corneal pachymetry is the process of measuring the thickness of the cornea.A pachymeter is a medical device used to measure the thickness of the eye's cornea.It is used to perform corneal pachymetry prior to refractive surgery, for Keratoconus screening, LRI surgery [1] and is useful in screening for patients suspected of developing glaucoma among other uses.
The thickness is then calculated from the fringe spacing. The method has been used to measure corneal thickness in frog and human corneas. These measurements have been correlated with histologic and pachometer measurements of corneal thickness. A significant capability of this technique is to measure the thickness of optically opaque corneas.Academy Members-Only Access. This content is available only to Academy members. Join the American Academy of Ophthalmology and enjoy these exclusive benefits:. One-stop clinical education via the Ophthalmic News and Education (ONE) Network How is cornea thickness measured? Cornea thickness is typically measured using a device called a pachymeter, which uses ultrasound waves to determine the thickness of the cornea. What is the ideal cornea thickness for LASIK surgery? The ideal cornea thickness for LASIK surgery is typically considered to be at least 500 microns.
Resultado da Check apkkill.com with our free review tool and find out if apkkill.com is legit and reliable. Need advice? Report scams Check Scamadviser!
corneal thickness is measured by|average corneal thickness range